Giant convexital meningioma of the right hemisphere of the brain: a clinical case
Авторы: Ткаченко Евгений Алексеевич, Эльканов Руслан Артурович, Спиридонова Елизавета Алексеевна, Дерябин Алексей Сергеевич, Раевская Анастасия Игоревна
Рубрика: 9. Медицина и фармакология
Опубликовано в
LII международная научная конференция «Исследования молодых ученых» (Казань, январь 2023)
Дата публикации: 11.01.2023
Статья просмотрена: 20 раз
Библиографическое описание:
Giant convexital meningioma of the right hemisphere of the brain: a clinical case / Е. А. Ткаченко, Р. А. Эльканов, Е. А. Спиридонова [и др.]. — Текст : непосредственный // Исследования молодых ученых : материалы LII Междунар. науч. конф. (г. Казань, январь 2023 г.). — Казань : Молодой ученый, 2023. — С. 17-22. — URL: https://moluch.ru/conf/stud/archive/474/17719/ (дата обращения: 05.05.2024).
The paper presents a clinical observation of successful surgical treatment of a patient with giant convexital meningioma of the right hemisphere of the brain.
Key words: meningioma, tumor, brain, neurosurgery, clinical case.
Meningioma is the most common primary intracranial tumor in adults and is more common in middle-aged women [1]. Although most meningiomas are encapsulated and benign tumors with a limited number of genetic aberrations, their intracranial location often leads to serious and potentially fatal consequences [2].
Classification of tumors of the central nervous system of the World Health Organization (WHO) from 2016 divides meningiomas into three degrees: I — slowly growing tumors, II — atypical meningioma, III — anaplastic or malignant meningioma. Among them, grade II and III meningiomas are associated with a high recurrence rate and premature mortality [1].
The average annual incidence rate is 7.86 cases per 100,000 people. There has been an increase in this indicator over the past 30 years, which may be associated, on the one hand, with earlier diagnosis and an increase in life expectancy, and, on the other hand, with a true increase in the incidence [3].
The material for this study was a clinical observation of a giant convexital meningioma of the right hemisphere of the brain.
Clinical case
Patient A, 50 years old. She was hospitalized in the neurosurgical department of a multidisciplinary hospital. At the time of admission, he complained of a moderate headache of a diffuse nature without a clear daily dependence, severe visual impairment, sleep disturbance, memory loss. It is difficult to name the time frame for the appearance of the first symptoms. Anamnesis of life without features.
Objectively at the time of admission: the condition is satisfactory. The position is active. Asthenic build, weight 60 kg, height 170 cm. BMI 20.76. Skin and visible mucous membranes of physiological color. Peripheral lymph nodes are not palpable. Vesicular breathing is heard over the entire surface of the lungs, there are no wheezing. The frequency of respiratory movements is 17 per minute. The heart sounds are clear, the rhythm is correct. Heart rate — 69 per minute, blood pressure — 130/85 mm Hg. The abdomen is soft on palpation, without pain. The spleen is not palpable. Shchetkin-Blumberg's symptom is negative. The symptom of «tapping» in the lumbar region is negative. Urination is independent. Chair is normal.
Neurological status: clear consciousness. 15 on the Glasgow Coma Scale. Memory and attention are reduced. In time and place she is disoriented, in her own personality and situation she is oriented. The answers to the questions are partially correct. Speech and the ability to operate with numbers are not impaired. There is a mild cognitive deficit. There are no meningeal symptoms. Cranial nerves: palpebral fissures, pupils, evenly expressed, photoreactions are preserved, the face is without gross asymmetry, the tongue is in the midline, swallowing is not disturbed. Paresis, pathological foot signs, gross sensory disorders were not revealed at the time of examination. Performs coordinating tests satisfactorily, stable in the Romberg position. Pelvic functions are controlled.
The patient underwent additional laboratory and instrumental studies.
In blood tests, leukocytosis (13.3 x 10 9 /l), an increase in the content of C-reactive protein (39.7 mg/l) and fibrinogen (5.72 g/l) are noted.
Magnetic resonance imaging of the brain reveals signs of a mass formation of the frontal lobe on the right with a mass effect and expansion of the contralateral lateral ventricle (Figure 1–3).
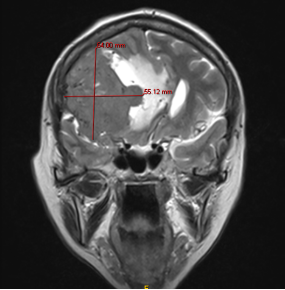
Fig. 1. MRI of the brain. Signs of convexital meningioma in the right fronto-parietal-temporal region (T2 mode, frontal plane)
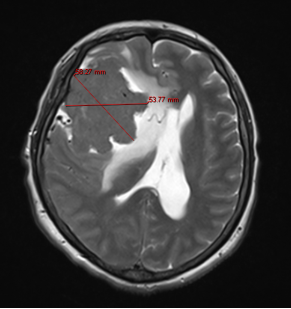
Fig. 2. MRI of the brain. Signs of convexital meningioma in the right fronto-parietal-temporal region (T2 mode, axial plane)
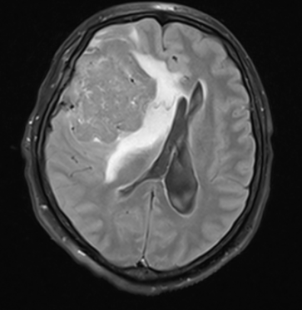
Fig. 3. MRI of the brain. Signs of convexital meningioma in the right fronto-parietal-temporal region (T2-FLAIR mode, axial plane)
Psychiatric consultation, conclusion: organic delusional disorder in the stage of unstable remission. Consultation of a neuro-ophthalmologist, conclusion: atrophy of the optic nerves of both eyes.
On the basis of complaints, additional examination data, the diagnosis was made: giant convexital meningioma of the right hemisphere of the brain. A decision was made to proceed with surgery.
After performing anesthesia, the patient was placed in the supine position with the head turned to the left by 30 degrees and fixed in the Mayfield bracket. Made C-shaped incision of soft tissues in the right fronto-parietal-temporal region. The skin-aponeurotic flap is retracted to the base. A craniotomy was performed in the right fronto-parietal-temporal region from five burr holes. The bone flap is raised and removed for the duration of the surgery. The dura mater (DM) is pulsating, moderately tense, sutured along the edge of the trepanation window. The DM was opened along the periphery with the definition of the boundaries of the tumor. Tumor tissue is devitalized. The tumor was removed in several large fragments and sent for histological examination. The degree of radicality Simpson I (macroscopically complete removal of the tumor with excision of the dura mater). Performed hemostasis. The plastic of the DM was performed with a free fragment of the periosteum. The skin flap was put in place and fixed with three titanium mesh fragments (Figure 4). Layered wound closure.
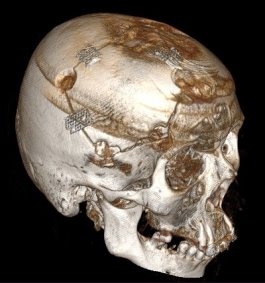
Fig. 4. Postoperative computed tomography of the head (3D reconstruction)
In the postoperative period, there is a positive trend in the form of a partial regression of cognitive impairment, improvement in visual functions.
The clinical interest of this observation lies in the importance of a multidisciplinary approach to the differential diagnosis of cognitive impairment in order to exclude organic causes of their development. A better understanding of this issue will ensure their early recognition and timely initiation of therapy.
Литература:
- Ugga L, Perillo T, Cuocolo R, et al. Meningioma MRI radiomics and machine learning: systematic review, quality score assessment, and meta-analysis. Neuroradiology. 2021;63(8):1293–1304. doi:10.1007/s00234–021–02668–0
- Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol. 2010;99(3):307–314. doi:10.1007/s11060–010–0386–3
- Thust S, Kumar A. Cham: Springer International Publishing. Extra-axial tumors. Clinical Neuroradiology, 2019;1115–1150